Introduction Hydroxyurea (HU) is worldwide used in the current clinical practice as first line treatment in high risk patients with Polycythemia Vera (PV). However, its efficacy has been seldom evaluated in the real-life setting.
Aims The present study aims to address the role of Complete Peripheral Recovery (CPR) as useful response criteria in PV patients treated with HU in a large cohort of unselected patients.
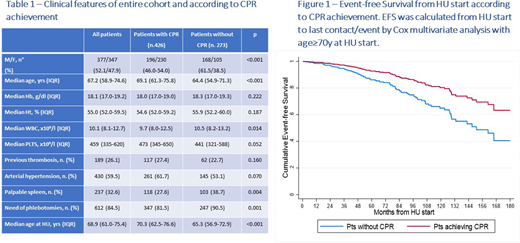
Methods After IRB approval, data of 846 PV patients, revised according to WHO2008/2016 and followed in 21 European Hematology Centers, were retrospectively collected. Definition of CPR during HU treatment included all the following criteria: hematocrit (Ht) level ≤45% (≤3 phlebotomies per year allowed), white blood cells (WBC) count ≤10 x109/l, platelets (PLT) count ≤ 400 x109/l. Spleen size and symptoms were not considered in the definition of CPR. Event-free survival (EFS), considering as event evolution into blast phase (BP) or myelofibrosis (MF) and death from any cause, was calculated from HU start to last contact/event by Cox analysis with age≥70y. Overall survival (OS) was calculated from the start of HU to last contact/death (log-rank p).
Results Among the 846 patients of the entire cohort, 724 (85.5%) were treated with HU after a median time from PV diagnosis of 2.6 months [interquartile range (IQR) 0.5 - 19.6]: the main clinical features of these 724 patients at diagnosis are reported in the Table 1.
Starting doses of HU, available in 709 patients, were <500 mg/day in 42 (5.9%), 500 mg/day in 371 (52.3%), 750 mg/day in 39 (5.5%), 1000 mg/day in 219 (30.9%) and >1000 mg/day in 38 (5.4%). Twenty-five patients were not evaluable for response to HU. Among the remaining 699 patients, 426 (60.9%) achieved a CPR after a median time from HU start of 4.9 months (IQR 2.1 - 15.7) while 273 (39.1%) never achieved a CPR. Among the 426 patients who achieved CPR, 115 (26.9%) needed a treatment period >12 months before obtaining the CPR. The main baseline clinical features of patients achieving or not CPR are reported in the Table 1: female sex, older age at diagnosis and at HU start, lower WBC count, no phlebotomies need and no palpable spleen were all associated in univariate analysis with CPR achievement.
During HU treatment, a thrombotic episode occurred in 36 patients achieving CPR (8.4%) compared to 16 patients without CPR (5.8%) (p=0.162). Among 426 patients achieving CPR, 20 (4.6%) evolved in MF and 10 (2.3%) evolved in BP: among 273 patients without CPR, 20 (7.3%) evolved in MF and 9 (3.3%) evolved in BF (p=0.134 and 0.451, respectively). Ten-year EFS was 79.2% [95%Confidence Interval (CI) 72.1 - 84.8] in patients achieving CPR compared to 67.3% (95%CI 56.9 - 75.7) in patients without CPR (p=0.001) (Fig. 1). Ten-year OS was 80.5% (95%CI 73.9 - 87.1) in patients achieving CPR compared to 74.4% (95%CI 65.6 - 83.2) in patients without CPR (p=0.116).
Conclusions In the current clinical practice, HU is effective in inducing CPR in about two thirds of patients with PV treated front-line. CPR is more frequently achieved by patients with lower disease burden, including lower WBC count, and less frequent PHL need and palpable spleen. Notably, >25% of responding patients achieved CPR after >12 months from HU start, suggesting the need for a long period of HU therapy before efficacy evaluation. The clinical importance of CPR is highlighted by a significantly longer EFS in patients achieving this type of response.
Breccia:Abbvie: Consultancy; Bristol-Myers Squibb/Celgene: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; Incyte: Consultancy, Honoraria; Novartis: Consultancy, Honoraria. Benevolo:Amgen: Honoraria; Celgene: Honoraria; Novartis: Honoraria. Cavazzini:Pfize: Honoraria; Incyte: Honoraria; Novartis: Honoraria. Heidel:Novartis: Consultancy, Honoraria, Research Funding. Crugnola:Novartis: Honoraria; Celgene: Honoraria; Janssen: Honoraria; BMS: Honoraria. Pane:AbbVie: Consultancy, Other: Travel Expenses, Speakers Bureau; Amgen: Consultancy, Other: Travel Expenses, Speakers Bureau; Daiichi Sankyo: Consultancy, Other: Travel Expenses; Jazz Pharmaceuticals: Consultancy, Other: travel expenses, Speakers Bureau; Novartis pharma SAS: Consultancy, Other: Travel Expenses, Research Funding, Speakers Bureau; Janssen: Other: Travel Expenses; Bristol Myers Squibb: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Celgene: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Cuneo:Roche: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Abbvie: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Gilead: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Astra Zeneca: Honoraria; Janssen: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Krampera:Janssen: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees. Semenzato:Abbvie: Honoraria; Roche: Honoraria; Takeda: Honoraria. Cavo:Jannsen, BMS, Celgene, Sanofi, GlaxoSmithKline, Takeda, Amgen, Oncopeptides, AbbVie, Karyopharm, Adaptive: Consultancy, Honoraria. Palumbo:Amgen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Palandri:Novartis: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal